Neurological symptoms
Additional symptoms
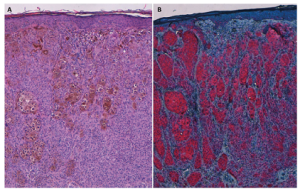
Picture: Pellegrini et al. Acta Derm Venereol 2020; 100: adv00040
Neurological symptoms
When melanocytosis does cause symptoms directly, they can come in different forms.
- Seizures are the most common complication. This symptom tends to occur most often when the melanin deposits are located in the temporal lobe. Seizures can be serious but are usually treatable. When a child has seizures, a neurologist (preferably pediatric) should be consulted. Seizures can often be successfully treated with medication. Some people have found success with epilepsy surgery, which removes a portion of the brain that is found to be causing the seizures.
- Hydrocephalus (too much fluid in the brain) – this symptom is caused by melanocytosis in the leptomeninges (the coverings of the brain and spine), which is not always visible on MRI. Hydrocephalus typically needs treatment with a special operation to shunt the fluid out of the brain. Signs of hydrocephalus in a baby include sunsetting eyes (the irises of the eyes seem to be sinking under the eye socket and only the top portion is visible), intractable or projectile vomiting, inconsolable crying, extreme sleepiness, bulging forehead or fontanel. Signs of hydrocephalus in an older child include intractable or projectile vomiting, severe or prolonged headache, and extreme sleepiness. If your child has nevi and is exhibiting any of these symptoms, he/she should be evaluated by a medical professional. Hydrocephalus can be successfully treated but it must be done without delay.
- Cysts or malformations of the brain, spinal syrinx, or tethering. Cysts or brain malformations can be found in people with NCM. Excess pigment cells in the spinal cord can cause syrinx, a fluid-filled cavity within the spinal cord. They can also cause tethering, which means that tissue attachments are limiting the movement of the spinal cord. Symptoms of these issues can include late bed wetting and toe walking. These behaviors can also be normal childhood issues but should be checked by a pediatrician or child neurologist if the child has nevi.
- Melanoma can occur in the brain. This complication is rare but can occur at any age.
Alarming symptoms
One should be vigilant for symptoms of developmental stagnation, among others. Alarming symptoms that require urgent referral include focal neurological abnormalities, epilepsy, increased intracranial pressure, or spinal cord compression.
In general terms, the occurrence of neurological symptoms in every patient with CMN, especially in a young child, should be a cause for great attentiveness and appropriate referral. The main alarming symptoms include neurological manifestations of:
- Focal abnormalities: e.g., especially epileptic seizures, movement disorders such as hemiparesis in case of abnormalities in the contralateral hemisphere.
- Increased intracranial pressure (hydrocephalus): e.g., headaches, vomiting, consciousness disorders; in very young children, the increased pressure can lead to an abnormally growing head circumference.
- Signs of spinal cord compression: e.g., a combination of gait disturbances, sensory disturbances in the legs, and issues with urination and defecation.
Mild symptoms
In addition to the above-mentioned alarming symptoms, milder neurological symptoms, such as developmental disorders, also deserve attention in children with CMN as they may indicate NCM. During the regular medical history (by a dermatologist), it is particularly important to inquire about subtle abnormalities, such as: overall development on schedule, performing well in school, and any unexplained deviations.
When an MRI
People with CMN can have differences in the brain or spinal cord called neurocutaneous melanocytosis (NCM). This means that excess
pigment cells (melanin) are present in the brain or spinal cord. The term neurocutaneous melanosis is not always used anymore because it is not specific enough. Differences can be detected on an MRI scan.
Many experts currently advise that any child born with two or more congenital melanocytic nevi (CMN) of any size or location should undergo a routine MRI scan of the brain and spine within their first year of life, ideally before reaching 6 months of age. While it cannot be ruled out that MRI abnormalities may occur in children with only one CMN at birth, the risk is significantly lower.
Should a child reach the age of two and remain in good health without having undergone a scan, it is unnecessary to retrospectively conduct the scan. Even if there were any anomalies, they would unlikely require intervention.
Why an MRI
MRI scan results fall into three main categories:
- Normal scan: This indicates a low likelihood of childhood melanoma, seizures, or significant neurodevelopmental issues. If problems arise, they are typically mild.
- Intraparenchymal melanosis only: Here, the chances of childhood melanoma are low, but there is some risk of seizures and neurodevelopmental problems.
- All other abnormalities on MRI scan: Individual cases will be evaluated by the medical team, but as a group, there’s a considerable risk of melanoma, the need for neurosurgery, seizures, and neurodevelopmental problems.
The MRI results serve as the most reliable predictor of potential clinical issues:
- Normal MRI: Children in this category do not require routine repeat scans or continuous developmental monitoring.
- Intraparenchymal melanosis only: Routine repeat scans are unnecessary, but regular developmental monitoring until school age is recommended. Early intervention for developmental support and establishing a school support plan should any issues arise is advised.
- All other abnormalities on MRI scan: Specialist management tailored to each individual case is recommended until the child’s condition stabilizes. Repeat scans may be necessary to monitor any changes, and there may be a need for neurosurgery. Regular monitoring of melanoma risk is also crucial.
In summary, the MRI results play a significant role in guiding the clinical management of children with CMN, ensuring appropriate interventions and monitoring are implemented based on the specific category of MRI findings.
Technique MRI
Dr. Barkovich specialized in high-resolution, state-of-the-art imaging to diagnose and treat neurological disorders in infants and children. He wrote the following paper on conducting an MRI for the neurological involvement of CMN.